Exercise in Post-acute COVID-19 Syndrome Patients: Fatty Acid Oxidation & Lactate Production
News Release, World Mitochondria Society, Berlin - Germany – March 21, 2022
After acute infection with the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), many individuals experience a range of symptoms including dyspnea, exercise intolerance, and chest pain commonly referred to as “post–COVID-19 syndrome” or as post-acute sequelae of SARS-CoV-2 infection (PASC). Exertional dyspnea and physical activity intolerance in PASC can be debilitating despite mild acute coronavirus disease (COVID-19) and normal resting pulmonary physiology and cardiac function.
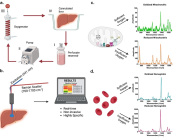
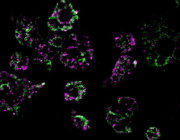
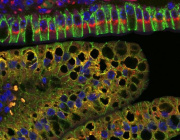
There is an urgent need to understand the pathogenesis of PASC and find effective treatments. The cardiopulmonary exercise test (CPET) is commonly used to investigate unexplained exertional dyspnea; as such, it could provide insight into mechanisms of PASC. CPET data can be used to calculate rates of β-oxidation of fatty acids (FATox) and of lactate clearance, providing insight into mitochondrial function. Fit individuals have better mitochondrial function and a higher rate of FATox during exercise than less fit individuals. In this study, they investigated whether patients with PASC had compromised mitochondrial function during graded exercise.
Data were obtained via retrospective review of the electronic medical record from a cohort of 50 subjects with PASC that were consecutively referred to and willing to complete CPET in the Pulmonary Physiology Laboratory at National Jewish Health between June 2020 and April 2021. Patients were assessed on a cycle ergometer using a continuous ramp protocol to exhaustion. Cardiovascular, ventilatory, metabolic, and gas exchange data were collected using a metabolic cart (Ultima Cardio2 System; Med graphics) per standard protocol. As a final step, patient data were compared with results from two published cohorts that included subjects tested with CPET in Denver, Colorado.
- Pulmonary function testing (PFT) showed mostly normal resting airflow and gas transfer capacity. All six patients (12%) with PFT abnormalities had preexisting illnesses, including asthma (n = 3) or interstitial lung disease. Resting transthoracic echocardiogram was obtained in 39 patients (78%) within 2 ± 3 months of CPET.
- Left ventricular systolic function was normal in all patients. Among the 50 patients who underwent CPET, the mean time from COVID-19 diagnosis to the CPET was 6 ± 4 months.
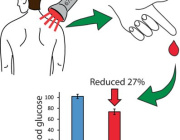
- Regardless of the presence of comorbidities, among the 39 patients with PASC who had arterial catheters in place, mean lactate was significantly higher; and in all 50 patients with PASC, calculated levels of FATox were significantly lower during exercise when compared with historical cohorts of subjects who are moderately active or with metabolic syndrome.
The data suggest that abnormally low FATox and altered lactate production by skeletal muscle as a putative cause of / contributor to the functional limitation of patients with PASC.
Normally, as glycolysis increases with exercise intensity, lactate is oxidized for fuel in mitochondria, mainly in adjacent slow-twitch muscle fibers. Like FATox, lactate clearance capacity is a useful surrogate for mitochondrial function. In patients with PASC, even in those with normal pre–COVID-19 physical fitness and free of comorbidities, the metabolic disturbances of the skeletal muscle during exercise may be worse than those reported in moderately active individuals or in individuals with metabolic syndrome. Whereas rising blood lactate levels are expected during high exercise intensity (as glycolytic flux exceeds the rate of mitochondrial pyruvate oxidation), a high blood lactate at lower exercise levels indicates mitochondrial dysfunction. The inappropriately high arterial lactate levels at relatively low exercise intensity in patients with PASC indicate that the transition from FATox to CHOox occurs prematurely, suggesting metabolic reprogramming and dysfunctional mitochondria.
This study provides the first evidence of mitochondrial dysfunction that advances our understanding of the pathogenesis of PACS in patients with preserved pulmonary and cardiac function. Future studies into the mechanisms of mitochondrial dysfunction in individuals with PACS will help accelerate the development of therapies to improve their functional status.
The implication of mitochondria in COVID-19 pathogenesis will be highlighted in Targeting Mitochondria 2022. If you have any studies that fit this title, you can submit your abstract now and share your work with the world mitochondria society.
© Image - kjpargeter, freepik
Media contact:
World Mitochondria Society
This email address is being protected from spambots. You need JavaScript enabled to view it.
+33-1-5504-7755
Targeting Mitochondria 2022 Congress
October 26-28, 2022 - Berlin, Germany
wms-site.com